I was encouraged to write this when I heard a listener on the radio ask a health professional how they would know they had a healthy gut. “Look at your poo!”, was the reply. Are you ready to do this?
(It’s an earthy colour this week.)
In one early blog, I featured the song clip “Everything Comes Down to Poo” from the old TV series Scrubs. Listen again to the lyrics.
Advertisers love to tell us how to keep our bowels regular. You must have seen ads targeting the over 55s having spoonfuls of fibre granules … which appear to miraculously keep you “going”, and happy enough to frolic outdoors the next day!
In ’60s and ’70s Singapore, “BMs” were a very serious subject. “How are your bowel motions?” was the first thing doctors asked patients. My mother chose to call them “big-ones”, and she wasn’t the only one.
“Did you do ‘big-ones’ today?”
If “Yes”: “Was it hard or soft?”
If “No”: “Wait till tomorrow – if it doesn’t come, I’ll give you Magnesia!”
But regardless of whether we “did” or “didn’t”, 6-month enemas were mandatory at Gran’s. Thankfully, she got tired of chasing me and we stopped after the second …
When I was 7, in Singapore’s General Hospital for a tonsillectomy, nurses greeted patients with “Did you do BM this morning?” I had to lie and say “Yes”, or they would return with a bedpan with that awful nozzle-and-bulb pink enema. These days, medical practitioners only ask if they think it’s relevant.
But did you know that even if our problem isn’t related to our colons, our stools give vital clues to our health?
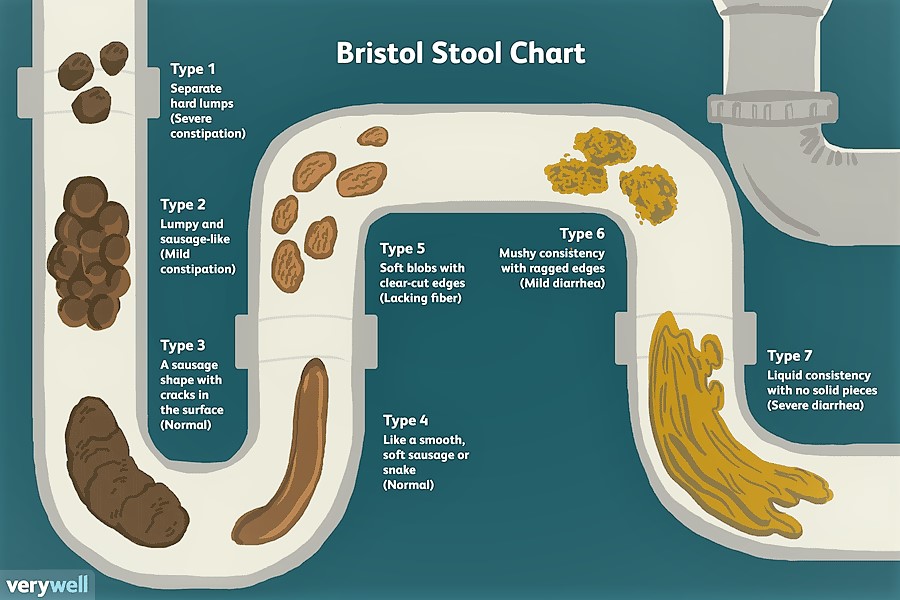
I later discovered the Bristol Stool Chart in the children’s book Your Growling Guts, which I highly recommend grown-ups read as well.
So – do you do Type 3 or 4? Or maybe 5, 6 or 7? And what’s the colour? Stools should be brown or slightly darker. If black, seek medical attention immediately.
(Always make sure your toilet bowl is white and clean beforehand, and only use clear toilet bowl cleaners).
I was a habitual psyllium-husk user and began to wonder why I suffered from “gas pockets”, identified as diverticulitis by my gastroenterologist. More psyllium was recommended which further aggravated my condition.
A few years ago, Anna Paredes from the Colonic Care Centre in Sydney suggested I stop the psyllium, have a green apple midday, and drink 2 ½ to 3 litres of water during the day. Much to my surprise, it worked and still does!
“I believe that more constipation is caused by not drinking enough water or eating enough citrus fruit than ever was caused by not getting enough bran in your diet.”
(Wills, J. (1990). “A flat stomach in 15 days“, p.28. Sphere Books Ltd: London.)
The apple-and-water regime may not give you the same results – but give it a try. A section of grapefruit or orange pith with the juice first thing in the morning certainly help. Walking and/or regular gym sessions are also wonderful “motion movers”.

Please re-consider the standard laxative options before stepping into the murky waters of that particular supermarket aisle:
- Oral ‘bulk- formers’: Usually usually in granule form, and include psyllium, chia and flax seeds. But you must drink enough water with them, or more constipation, discomfort and bloating will result.
- Oral stimulants and rectal suppositories (e.g. Milk of Magnesia, Epsom Salts and enemas): These trigger contractions of intestinal muscles to eliminate stools and often cause cramping and diarrhoea. Not for habitual use!
The Mayo Clinic has comprehensive and very useful information on laxatives and their side effects. And Dr Norman Walker sums it up in one sentence:
“In simple words the colon is the sewage system of the anatomy”.
(Walker, N.W. (1940/1970). Diet & Salad, p.11. Norwalk Press: Summertown, Tennessee.
Thank goodness for our efficient sewage system. But before flushing the evidence away at the quick press of a button, do VIEW YOUR POO!
To leave your comments, just click on this link and scroll to the end of the post.
